act early! screen early! - rasing awareness for pre-eclampsia 2023
May is Pre-eclampsia awareness month and 22nd May is World Pre-eclampsia Day: for the sixth time we want to raise awareness for this severe and dangerous pregnancy complication, and invite you to join us! Support our campaign “act early! screen early!”
How to join and support:
- Download and share the campaign materials you find below
- Be sure to use the hashtags #ActEarlyScreenEarly and #WorldPreeclampsiaDay2023
- Please tag @efcni or @EFCNIwecare on Twitter
Download our campaign material
We kindly invite you to read an insightful guest article authored by Sandra Walther from Frühchen Schweiz, who shares her personal experience with pre-eclampsia as an affected mother and kindly supports our Pre-eclampsia awareness campaign with her contribution.
Pre-eclampsia: symptoms, risk factors and risk assessment
Pre-eclampsia, sometimes also referred to as “toxaemia of pregnancy”, is a complication of pregnancy that affects approximately 2 out of 100 expectant women. The main symptoms for pre-eclampsia are elevated blood pressure and high protein levels in the urine. The condition can be very dangerous for both, mother and baby. Luckily, severe and early forms of pre-eclampisa (=<34 weeks’ gestation) are seldom. Regular antenatal care is however most important to enable the detection of the disease as early as possible.
Pre-eclampsia can develop into HELLP syndrome or eclampsia, with life-threatening complications for the mother ranging from organ damage to death if not treated quickly and competently. “HELLP” is an abbreviation for the three main symptoms of this syndrome: Haemolysis, Elevated Liver enzymes, and Low Platelet count.
What are the consequences for mother and baby?
Pre-eclampsia is one of the most common causes of preterm birth. It is also associated with a high risk of the baby being born too small and with a low birth weight, as the condition prevents the fetus from being adequately nourished and supplied with oxygen. There is a possibility that the baby may have problems with heart and circulatory conditions in later life.
Pre-eclampsia also might have long-term health effects for the mother. Over 90% of women with severe pre-eclampsia develop chronic high blood pressure 20 years after their pregnancy, and frequently suffer from cardiovascular diseases. Competent continuing care of both mother and child by an expert and a healthy lifestyle (such as a healthy diet, physical activity, avoiding stress) are particularly important in seeking to prevent them.
What are the risk factors?
A range of factors increase the risk of developing pre-eclampsia. These include
- a first pregnancy
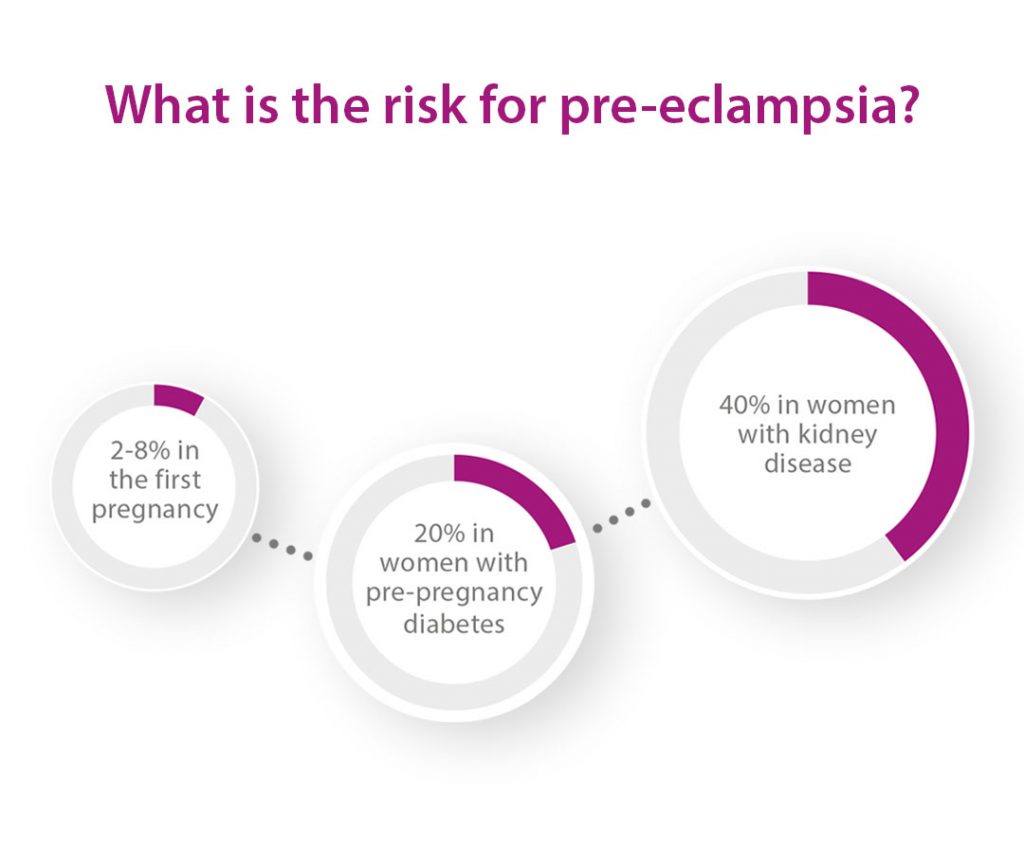
- a multiple pregnancy
- pre-eclampsia or fetal growth restriction in a
previous pregnancy or in the pregnancy of a relative - a pregnancy involving artificial insemination/egg donation
- pre-existing high blood pressure
- kidney disease
- diabetes
- overweight
- higher maternal age
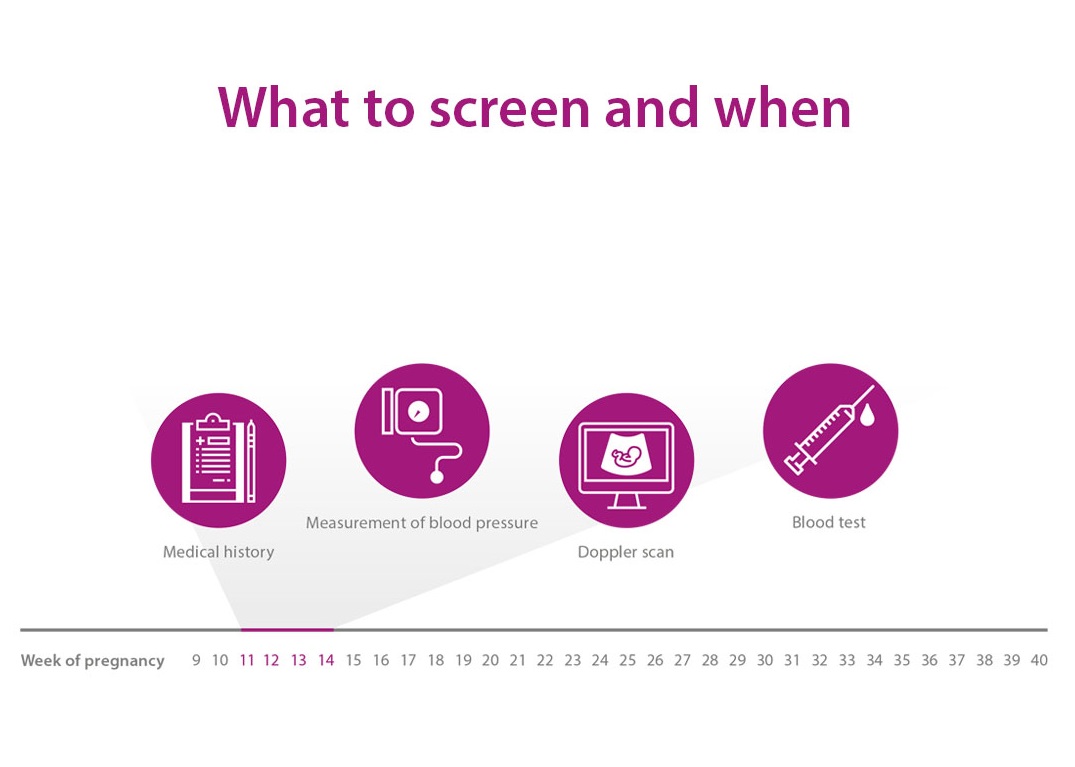
Pre-eclampsia screening in the first trimester
Pre-eclampsia is indicated by elevated blood pressure and increased protein excretion in the urine. Even if not recognisable from the outside, the disease originates already during the first trimester of pregnancy. The risk of developing pre-eclampsia should be detected as early as possible to take preventive measures. A test between 11 and 14 weeks of pregnancy can determine the individual risk of developing pre-eclampsia. This involves checking the blood pressure, performing a Doppler scan and taking a maternal blood sample for measuring specific proteins. The result of these tests indicate a high risk for pre-eclampsia long before any clinical symptoms appear.
If the test shows an increased risk, changes regarding diet and lifestyle as well as low-dose aspirin has to be prescribed by the responsible specialist. It can in particular decrease the risk of developing the early and most serious form or pre-eclampsia.
The earlier the risk of developing pre-eclampsia is known, the more likely it is to continue the treatment in a specialised centre.
How is pre-eclampsia diagnosed in later trimesters?
Additionally, a blood test in the second and third trimester analysing two placental proteins can predict the onset of pre-eclampsia about four weeks in advance. With this information, the frequency of antenatal care visits can be scheduled accordingly.
What can pregnant women do?
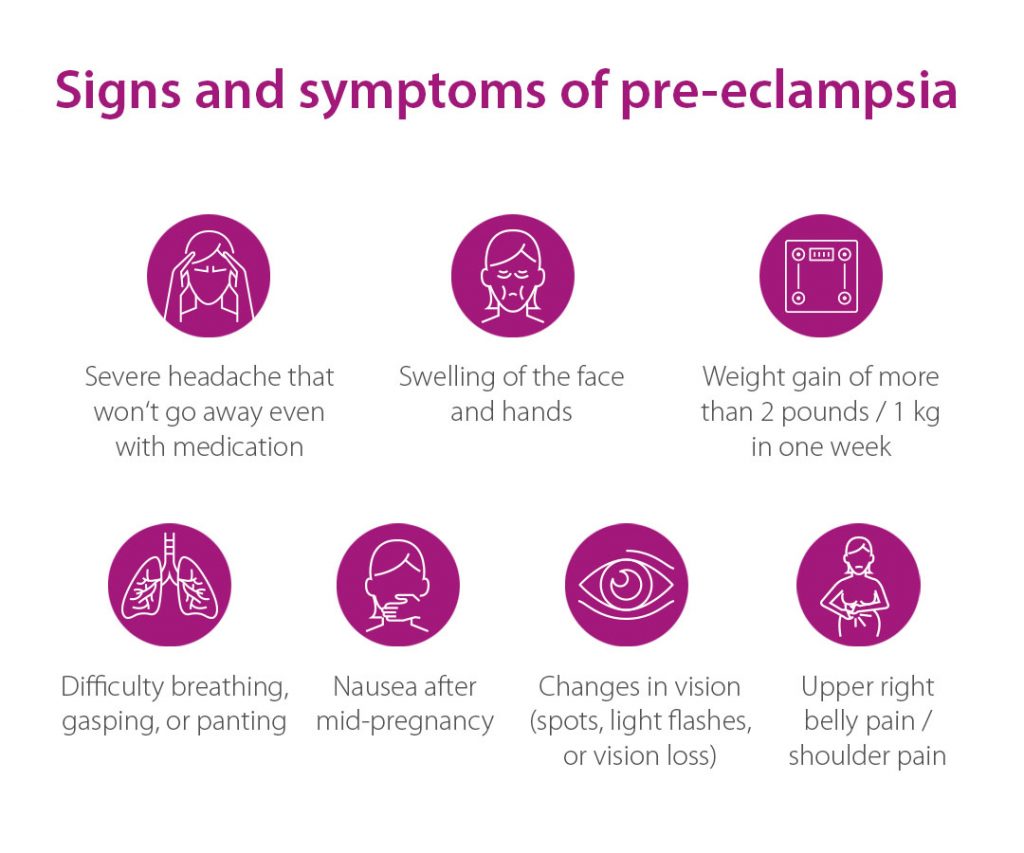
For pregnant women it is very important to keep every prenatal appointment. Additionally, regular self-monitoring of the blood pressure should be undertaken. In case of becoming aware of potential specific warning signals such as headaches, impaired vision, rapid weight gain (more than 1 kg per week), marked water retention in the body or restlessness, a physician must be seen immediately.
Monitoring and treatment of women with diagnosed pre-eclamspia
The only way to cure pre-eclampsia is to deliver the baby. However, prolongation of pregnancy to avoid a preterm birth is sought for as long as it is safe for mother and baby. Thus, women with pre-eclampsia must always be monitored by an expert, sometimes in a hospital setting.
Factsheet
Pre-eclampsia: further campaign material
Check out our YouTube Playlist for parental and expert statements on pre-eclampsia and pre-eclampsia prevention.
Partners and supporters
We warmly thank the following collaborating medical societies for supporting the campaign in 2023:

Our thanks go to the following patient – and parent organisations for supporting this campaign worldwide in 2023:

From 2017 to 2021, the topic of pre-eclampsia awareness and the campaign act early! screen early! were kindly supported by Thermo Fisher Scientific.