Pregnancy complications
Many infections are tested right in the beginning of pregnancy as part of the antenatal care package.
However, some infections can develop during pregnancy. Therefore, if a woman notices anything abnormal or does not feel well, it is good to see the responsible health professional right away, as infections can be treated easily and effectively if they are diagnosed in time.
A good example for an effective treatment if noticed early is a regular vaginal infection. Pregnant women should be aware of potential infections such as gastro-intestinal or urinary tract infections, viral infections such as cytomegalovirus (CMV), hepatitis or HIV (although relatively rare), sexually transmitted diseases such as chlamydia, but also blood-born diseases such as toxoplasmosis.
Vaginal infections
Vaginal infections are very common and the incidence increases even more during pregnancy. A vaginal infection may become dangerous if it is unrecognized and left untreated. In particular during pregnancy, hormonal fluctuations can quickly disrupt the pH balance of the vaginal environment. The pH balance, however, provides a natural barrier against harmful bacteria. A pH balance below 4.5 indicates that certain types of bacteria are multiplying in the vagina that may cause preterm labour.
How can a vaginal infection be prevented?
These days, regular pH monitoring of the vagina can be easily done using self-testing pH indicators. With their help, the woman can test her current pH balance by comparing the colour of the used indicator with a provided coloured scale. If she notices that the colours are different and thus the pH balance might be disturbed, it is good to wait a couple of hours to test again. Certain factors might influence the test, such as if urin accidently touches the indicator or if recent intercourse has occured. If the indicator stripe remains the same colour after a second test, a health professional should be consulted to prevent a vaginal infection from developing.
CMV - Cytomegalovirus
The cytomegalie infection is the most common congenital virus infection, even more common than rubella and toxoplasmosis. The virus is widespread all around the world. Whereas the prevalence of CMV-positive people in developing countries is about 100%, in Europe, the numbers vary from 30% to 100%.Usually, the CMV infections in healthy children and adults occur without noticing and without any health impairment. In rare cases only, there are temporary flu-like symptoms. A lack of knowledge of one’s own CMV immune status bears a risk for the unborn child. Through some simple information about possible causes of infection or ways of transmission, pregnant women can protect themselves from a primary infection.
If the mother becomes primarily infected during pregnancy, the immune system of the fetus cannot cope with the virus yet. Severe disease symptoms may appear that will later become manifest in a chronic course.
The transmission from mother to child
When a CMV-negative woman catches the virus for the first time during pregnancy, it can be transmitted via the placenta to the baby. This can have tremendous consequences for the infant. Some children show symptoms right after birth, such as hearing or speech disorders. Another consequence is a mental impairment with a permanent IQ below 70 whereas the mother’s infection will mostly pass unnoticed.
However, a large number of affected newborns whose mothers got infected during pregnancy do not show any symptoms. This is called asymptomatic progression. Approximately 8 percent of these children, however, will develop deficits at a later date.
Protective measures for seronegative women during pregnancy
- good hand hygiene with water and soap
- no joint use of knives, forks, spoons, etc. with any persons in one’s own environment
- no mutual exchange of food covered with saliva
- strict avoidance of kisses on the mouth
- avoid contact with persons who are presently infectious
- infants below three years of age can excrete the CMV virus via urine and saliva. Attention should be paid during diaper changes (wearing gloves), with toys, etc.
- testing of the partner
Some countries have different rules and regulations for certain occupational groups, such as educators and health professionals implemented. This can include an employment ban if dealing with children under the age of three, for instance; or an examination of safety at work with regard to the immune status.
CMV and preterm infants
In case of a preterm birth, the CMV status of the mother plays a crucial role in breastfeeding. Below 32 weeks of pregnancy, the CM virus can be transmitted through the breast milk and infect the preterm infant, if the mother is CMV-seropositive, meaning that she carries the virus inside her. Breastmilk, however, is the best nutrition for preterm infants and can help a lot to improve morbidity and mortality. Many hospitals thus still try to use the breastmilk to feed very preterm babies. Pasteurization is one way of making breastmilk safe for preterm infants. The disadvantage, however, is the elimination of all antibodies and lymphocytes in the breastmilk. Freezing significantly reduces the CMV viral load in breast milk and may also reduce the risk of infection, but may not eliminate it completely.
Toxoplasmosis
Toxoplasmosis is an infection caused by a common parasite called Toxoplasma gondii. Many animals, such as sheep, cattle, cats and dogs but also humans, can be infected with this single-celled parasite.It is considered to be an under-detected and underreported disease in the European Union. People can aquire a toxoplasmosis infection through following ways:
- by eating raw meat or unwashed vegetables and salad that is contaminated
- through contact with faeces particularly of cats
An infection with the parasite is usually without or mild symptoms, such as those of a mild flu.
Congenital toxoplasmosis
If a woman who has not had a toxoplasmosis infection is infected shortly before or during pregnancy, she can pass it on to her baby who is then born with toxoplasmosis (known as congenital toxoplasmosis). Depending on when in pregnancy the infection was aquired, the symptoms of the baby will vary. Symptoms include hydrocephalus, brain damage, epilepsy, jaundice, deafness, eye infections and reduced vision, growth problems, or even cerebral palsy.
During early stages of pregnancy the infection can lead to miscarriage and stillbirth. The later in pregnancy the mother is infected, the more likely that the baby does not have any severe symptoms. However, complications can still develop later in life of the child.
The chance of the baby being infected also varies with gestational age. The risk of the baby being infected with toxoplasmosis is less than 5% during the time of conception but increases to up to 65% risk of infection in the third trimester.
Prevention
The easiest way of preventing the child to become infected is to take preventive measures.
These include:
- regular hand washing
- avoiding emptying the cat litter or wearing gloves while handling with cat faeces
- wearing gloves when gardening
- thorough washing of salad and vegetables, and
- no consumption of raw meat or unpasteurized goat milk products
Many women who want to have a baby suffer from chronic diseases. In some cases, they are not necessarily aware that they are ill—many diseases allow us to lead a very normal life without being restricted in any way. Nevertheless, it is important to receive counselling, care and, if necessary, treatment for some diseases before becoming pregnant to ensure a normal pregnancy and a healthy start in life for the baby.
Asthma
Asthma is the most common chronic disease occurring in the first half of life. If a pregnant woman has an asthma attack, her oxygen supply and possibly also that of her unborn child may be compromised. However, with proper medical care and medication, no complications should arise during pregnancy or birth.
Diabetes
In Europe, about 35 million adults have diabetes. Diabetes causes elevated blood glucose levels. These days, a woman with diabetes can have a healthy baby just like anyone else, provided that she receives the best possible care and controls her blood glucose levels before becoming pregnant. However, it is essential that the pregnancy is carefully monitored: this means regular self-checks of maternal blood glucose levels and an adequate care together with a diabetes expert, i.e. a diabetologist. Blood glucose level should be optimal for at least three months before becoming pregnant. For diabetic women there is, however, still a slightly higher risk of developing pregnancy complications.
Gestational diabetes
About 5-10% of women suffer from gestational diabetes during their pregnancy. This type of diabetes occurs for the first time during pregnancy and normally disappears afterwards. Women with this disease are often unaware of it. Many countries offer a glucose intolerance test as part of the antenatal care programme to detect gestational diabetes.
Thyroid disorders
The thyroid gland regulates the production of many hormones in the human body and therefore affects our metabolism as a whole. Thyroid dysfunction during the early weeks of pregnancy may result in problems for the child, in particular during the early years of life. With this disease, too, it is important to receive diagnosis and treatment by a doctor as early as possible—ideally before becoming pregnant.
High blood pressure
Elevated blood pressure can often be regulated by taking a number of simple steps. With appropriate medication and care, women with (chronic) high blood pressure can enjoy their pregnancy, but should take things easier and, above all, avoid stress.
Pregnant women with elevated blood pressure belong to a high-risk category, and therefore require additional medical supervision by a specialist throughout the entire pregnancy. This is especially important to detect early signs of complications such as pre-eclampsia.
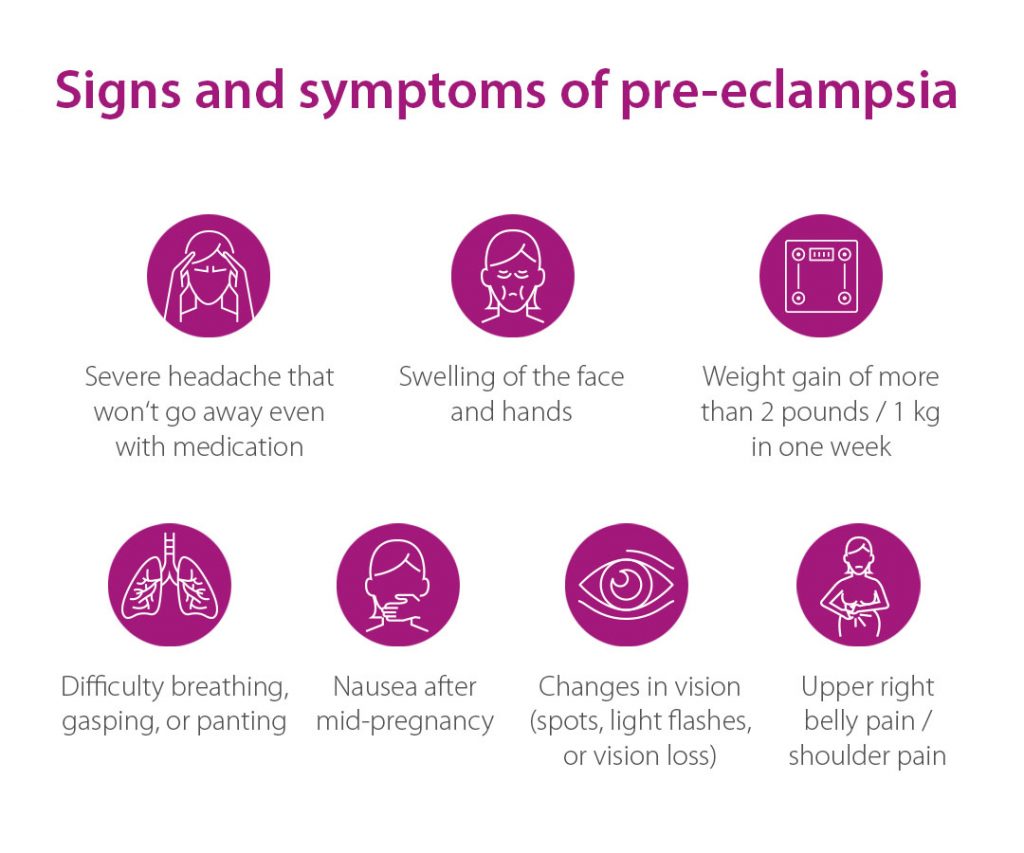
Pre-eclampsia, sometimes also referred to as “toxaemia of pregnancy”, is a complication of pregnancy that affects approximately 2 out of 100 expectant women. The main symptoms for pre-eclampsia are elevated blood pressure and high protein levels in the urine. The condition can be very dangerous for both, mother and baby. Luckily, severe and early forms of pre-eclampisa (=<34 weeks’ gestation) are seldom. Regular antenatal care is however most important to enable the detection of the disease as early as possible.
Pre-eclampsia can develop into HELLP syndrome or eclampsia, with life-threatening complications for the mother ranging from organ damage to death if not treated quickly and competently. “HELLP” is an abbreviation for the three main symptoms of this syndrome: Haemolysis, Elevated Liver enzymes, and Low Platelet count.
What are the consequences for mother and baby?
Pre-eclampsia is one of the most common causes of preterm birth. It is also associated with a high risk of the baby being born too small and with a low birth weight, as the condition prevents the fetus from being adequately nourished and supplied with oxygen. There is a possibility that the baby may have problems with heart and circulatory conditions in later life.
Pre-eclampsia also might have long-term health effects for the mother. Over 90% of women with severe pre-eclampsia develop chronic high blood pressure 20 years after their pregnancy, and frequently suffer from cardiovascular diseases. Competent continuing care of both mother and child by an expert and a healthy lifestyle (such as a healthy diet, physical activity, avoiding stress) are particularly important in seeking to prevent them.
What are the risk factors?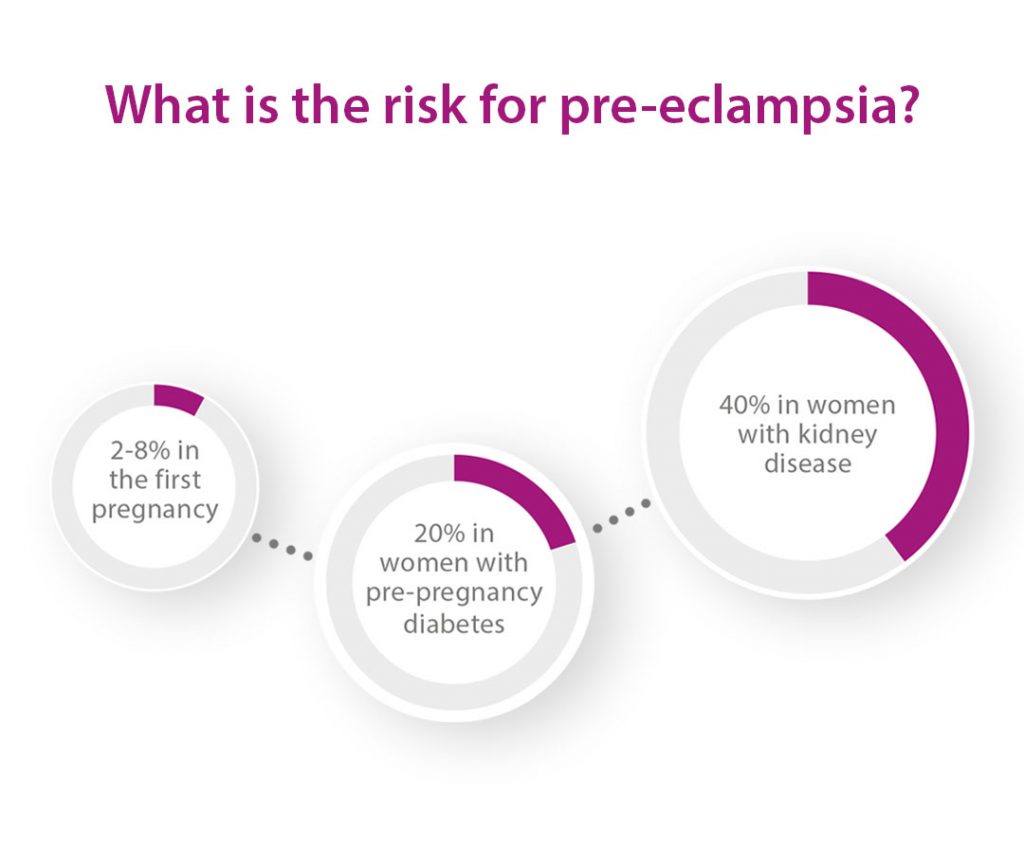
A range of factors increase the risk of developing pre-eclampsia. These include
- a first pregnancy
- a multiple pregnancy
- pre-eclampsia or fetal growth restriction in a
previous pregnancy or in the pregnancy of a relative - a pregnancy involving artificial insemination/egg donation
- pre-existing high blood pressure
- kidney disease
- diabetes
- overweight
- higher maternal age
Pre-eclampsia screening in the first trimester
Pre-eclampsia is indicated by elevated blood pressure and increased protein excretion in the urine. Even if not recognisable from the outside, the disease originates already during the first trimester of pregnancy. The risk of developing pre-eclampsia should be detected as early as possible to take preventive measures. A test between 11 and 14 weeks of pregnancy can determine the individual risk of developing pre-eclampsia. This involves checking the blood pressure, performing a Doppler scan and taking a maternal blood sample for measuring specific proteins. The result of these tests indicate a high risk for pre-eclampsia long before any clinical symptoms appear.
If the test shows an increased risk, changes regarding diet and lifestyle as well as low-dose aspirin has to be prescribed by the responsible specialist. It can in particular decrease the risk of developing the early and most serious form or pre-eclampsia.
The earlier the risk of developing pre-eclampsia is known, the more likely it is to continue the treatment in a specialised centre.
How is pre-eclampsia diagnosed in later trimesters?
Additionally, a blood test in the second and third trimester analysing two placental proteins can predict the onset of pre-eclampsia about four weeks in advance. With this information, the frequency of antenatal care visits can be scheduled accordingly.
What can pregnant women do?
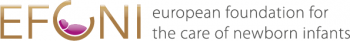
For pregnant women it is very important to keep every prenatal appointment. Additionally, regular self-monitoring of the blood pressure should be undertaken. In case of becoming aware of potential specific warning signals such as headaches, impaired vision, rapid weight gain (more than 1 kg per week), marked water retention in the body or restlessness, a physician must be seen immediately.
Monitoring and treatment of women with diagnosed pre-eclamspia
The only way to cure pre-eclampsia is to deliver the baby. However, prolongation of pregnancy to avoid a preterm birth is sought for as long as it is safe for mother and baby. Thus, women with pre-eclampsia must always be monitored by an expert, sometimes in a hospital setting.
For more information on pre-eclampsia such as causes, prevention, and the diagnosis after week 20 of pregnancy, please download our new factsheet that is available in Dutch, English, French, German, Greek, Hebrew, Hungarian, and Russian.